Right Place. Right Time.

The young assistant professor was studying an unremarkable virus called Zika when UNC brought her into its formidable infectious disease research community.
by Janine Latus
The Zika virus was what you might call a side project for Helen Lazear.
Insect-borne viruses that circulate between insects and monkeys in the jungle —and that generally cause no significant harm to humans — that’s Lazear’s main area of study.
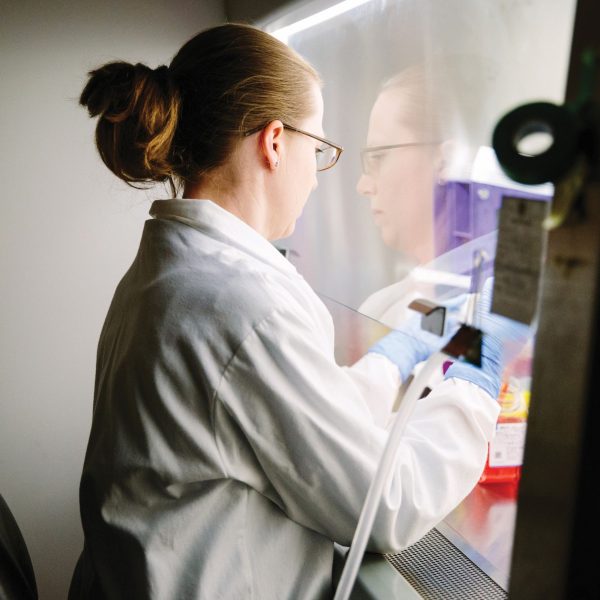
Helen Lazear studied the Zika virus in her postdoctoral work as part of the routine exploration of viruses in its family. Now in her lab in the Burnett-Womack Building at UNC, the research has taken on more urgency. (Photo by Anna Routh Barzin ’07)
In her postdoctoral work at Washington University in St. Louis, Lazear thought about which of these viruses were good candidates for emergence into a wider outbreak. Which ones, for example, were most likely to become a problem for people?
“Because these things don’t come from nowhere,” she says. “Usually you’ll have a scenario where there’s sort of a smaller simmering outbreak somewhere that maybe people who study these things are aware of, and it just hasn’t really gotten large enough that the wider world is paying attention.”
She set up systems to study such viruses in case an outbreak occurred. The work, which she hurried to finish before leaving her postdoc, included what she called “a ton” of Zika virus experiments.
Zika is not new. It was discovered in 1947 in Uganda, and named for a forest there. It’s moved around: Where people go, so go disease-carrying mosquitoes. It caused fever and rash in adults, but they recovered easily. Not exactly a public health emergency; still, understanding it would help Lazear understand other viruses.
In 2007, Zika cases emerged in Asia, then on several Pacific islands. In spring 2015, it showed up in Brazil. Six months later, that country told the World Health Organization about an unusual spike in cases of microcephaly — a birth defect, considered rare, in which a newborn’s head is significantly smaller than it should be. Two weeks later, health officials in Brazil spotted a connection.
That was about the time UNC Assistant Professor Helen Lazear, then 34, was opening her lab in the department of microbiology and immunology. She’d come to one of the country’s foremost places to study infectious disease just as the Zika virus was shifting from side project to front-page news.
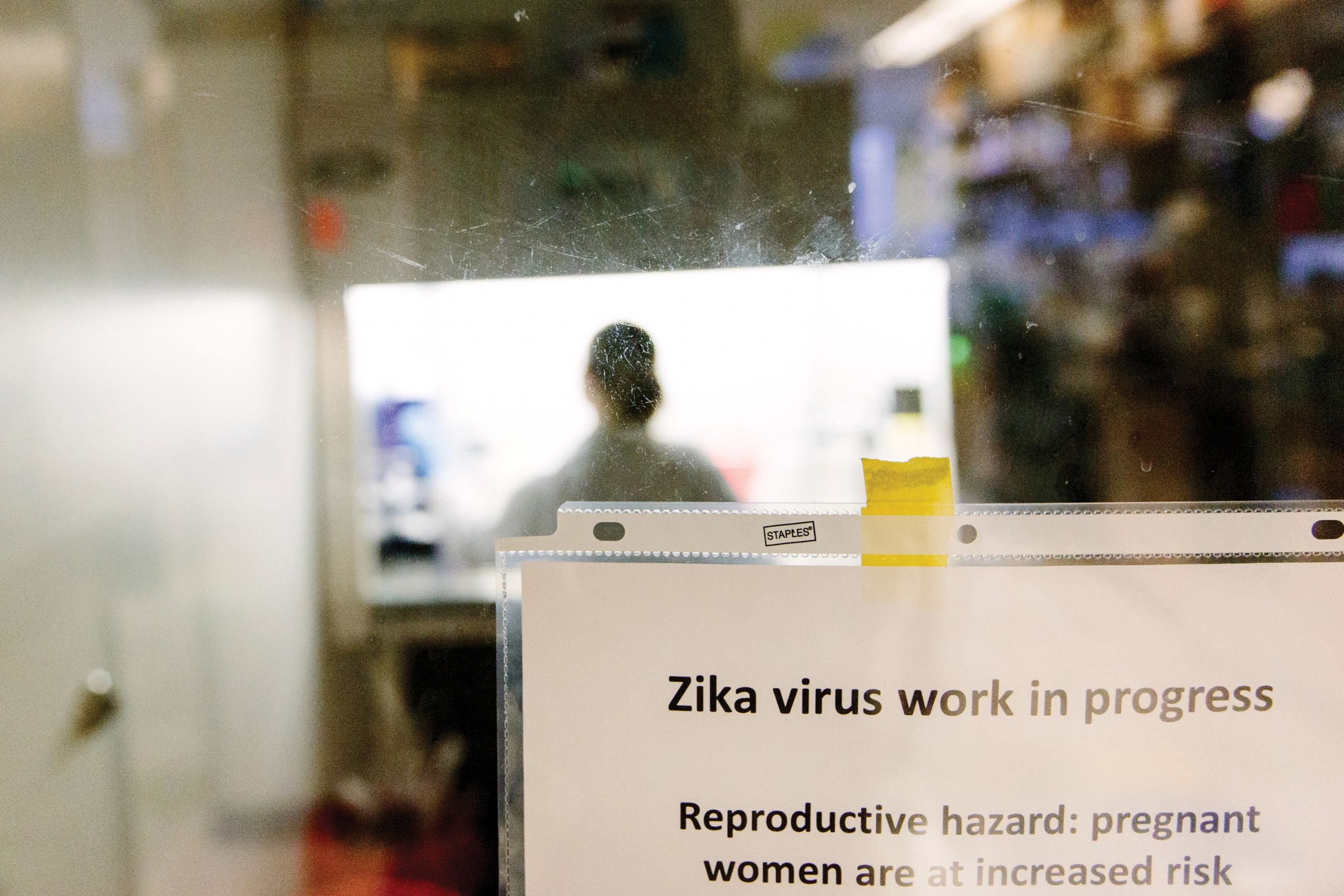 The usually routine discussions with UNC’s institutional biosafety committee — which deals with how to protect lab workers from nasty stuff they work with — weren’t just academic this time: Lazear, whose lab was gearing up to handle the Zika virus daily, was pregnant with her third child.
The usually routine discussions with UNC’s institutional biosafety committee — which deals with how to protect lab workers from nasty stuff they work with — weren’t just academic this time: Lazear, whose lab was gearing up to handle the Zika virus daily, was pregnant with her third child.
“Starting a new lab is always a challenge,” she said. “Starting a new lab when there’s an outbreak on the disease that you work on is exciting but especially challenging — it brings new opportunities but also a lot of competition. Also, I was pregnant while I was doing all of this. It turns out that the disease causes birth defects. So that was a whole extra level of intensity on it.”
There’s no more dwelling on that. Her son was born healthy in June, and Lazear’s thoughts are with Zika-infected mothers who weren’t so fortunate.
More questions than answers
“There certainly are other viruses that cause birth defects — that’s known,” Lazear said, “but this group of viruses are just not associated with that. To people who were familiar with this field, it was very surprising, and I think there was a lot of skepticism early on — myself included — that perhaps there was something else going on or some other factors having a role there.”
So Lazear turned her full focus onto Zika, particularly on the core questions of how it invades compartments that usually are safe — the placenta, the brain, the testes — all of them off limits to most pathogens because of the body’s protective barriers. The Zika virus is particularly alarming because it can invade all three. It is a medical crisis as well as a scientific anomaly. Lazear explains:

Lazear was pregnant with her son, Nate, when she started Zika research at UNC. (Photo by Anna Routh Barzin ’07)
“The developing fetus has a number of mechanisms that protect it from pathogens in the mother. And it turns out that the immunological responses during pregnancy are very sophisticated and quite fascinating. So, for the most part, the placenta forms a barrier that protects the fetus from pathogens in the mother. Most pathogens are not able to access the fetal compartment.
“The fact that there is a fairly discrete list of pathogens that are able to cross the placenta and access the fetus tells you there aren’t very many organisms that can do this. Zika can. And we don’t really understand how that is or what’s different about Zika virus that allows it to access the fetus when other related viruses don’t.
“The second thing is the ability of the virus to cause damage to the fetus once it’s there.”
Lazear’s research is both basic and complex. Her researchers measure viral infections in different cell types. They infect mice and watch what happens, then take tissue out to see how much virus is in various organs. They manipulate the viral genome to see which switch allows it to enter the brain, and they alter the mice’s genetic makeup to see which parts of the immune system are most protective.
If researchers use formaldehyde on the mice, the virus dies, so they can’t measure the virus’s ability to grow, but they can take tissue slices and look for the viral genome or proteins to determine where it’s been. Maybe there’s a protein they think is important for tightening the barrier into the fetal compartment or the brain and prevents the virus from getting through.
Because Zika hadn’t been associated with birth defects in past outbreaks, it’s possible that there are differences in the virus circulating in the Americas, or there may be differences in the genetic makeup or immunity of the host population. Or perhaps it was causing birth defects all along and previous outbreaks were so small that it wasn’t detected. As in so much of infectious disease research, questions far outnumber answers, but the expediency is clear.
“The stakes are pretty high when you’re talking about being able to cause birth defects,” Lazear said.
When Zika enters the fetal brain, it can disrupt the development of neurons, so the brain fails to develop. In some cases, it can cause loss of vision or hearing or can result in improperly developed joints.
“I think we’re only just beginning to learn about this spectrum of defects that the virus can cause, and we really don’t yet understand exactly why those are happening and what tissues are getting affected and how the virus causes this damage. We don’t understand what are the stages of gestation where the virus is more likely to spread from the mother to the fetus and where it’s more likely to damage the fetus.
“There are a lot of unknowns, and it’s difficult because — of course — pregnant women and families, they want to know: ‘When is my baby vulnerable? When can I know that we’re safe?’
“And we don’t have good answers.”
The race to solutions

Aravinda de Silva (Photo by Anna Routh Barzin ’07)

Stefan Metz (Photo by Anna Routh Barzin ’07)
Lazear’s lab abuts that of Aravinda de Silva, a professor of microbiology and immunology in the School of Medicine who studies the Dengue virus. Dengue accounts for hundreds of millions of infections worldwide every year. Dengue also is Zika’s closest cousin; it does not cause birth defects.
The research into one virus informs the other. Stefan Metz, a postdoctoral fellow in microbiology and immunology, is building on a Dengue vaccine platform in de Silva’s lab to create a nanoparticle-based vaccine for Zika. Instead of using a whole, replicating virus in the vaccine, which in Dengue has caused serious side effects, Metz is using just the portion of a protein from the surface of the Zika virus that sparks an immune response in people. By leaving out the rest, he thinks he can make a vaccine that’s far safer.

Ralph Baric (Photo by Anna Routh Barzin ’07)
Mark Heise (Photo by Anna Routh Barzin ’07)
One challenge in studying Zika is that it doesn’t infect mice very well, so UNC researchers in another lab are cataloging mice that better mimic the genetic diversity found in humans. The labs of Ralph Baric, a professor of epidemiology, microbiology and immunology in UNC’s Gillings School of Global Public Health, and Mark Heise, a professor of genetics in the medical school, are screening mice, each of which has a slightly different scrambled genome, to find the ones most susceptible to Zika.
“Humans are an outbred population,” Baric said. “We have mixed genes, so some of us are highly susceptible to a certain disease, and some highly resistant to one but then susceptible to another.”
So these researchers are finding lines of mice — most of them bred at UNC — that allow Zika to infect the brain or that let the virus through the placenta, or both. The more accurately the mouse model captures the vastly mixed genetics of the human population, the more efficiently it can be used to help humans.
Baric, using a database of genetic sequences from around the world to re-create earlier models of the Zika virus, aims to see when Zika morphed from being mostly benign into being dangerous. Knowing that will help speed development of treatments and vaccines, both ones that work against numerous related viruses and ones that work just against the current strain.
“Somewhere in that family tree, mutations occurred that made Zika more transmissible and pathogenic, especially to a developing embryo,” Baric said. “In that sequence lineage are the clues to how this occurred.”
And then a process that once took decades to work can take mere weeks.
“A new virus can emerge in China or Africa or the U.S., and the sequence can be available in two days,” Baric said. “Within a week, it can be placed into vaccines.”
Phase I Zika vaccine trials are available. But now Zika has thrown scientists another curve. Somehow it has become sexually transmittable. That is unprecedented.
“When the reports of sexual transmission started occurring, once again there was some skepticism,” Lazear said, “because we don’t see this with other related viruses.”
People in the U.S. have become infected even though they hadn’t been exposed to infected mosquitoes. Their partners had been exposed, though, so now the race is on to see how long Zika is present in semen. The testes are, after all, an immune privilege site, as are the brain and the fetal compartment. The human immune system doesn’t pay as much attention to them, so there’s evidence that the virus can linger, and men can spread the virus for a long time after their own infections have cleared.
“It’s problematic because you have someone who by all appearances has recovered, and yet we don’t know how long that can persist,” Lazear said.
So researchers are trying to predict who will shed virus for a long time and who will clear it quickly.

“Right now, we’re talking about Zika, but in a few years it’ll be something else,” Lazear says. (Photo by Anna Routh Barzin ’07)
A long way in a year
The University’s vast infectious disease network extends into the heart of the Zika outbreak.

Sylvia Becker-Dreps ’08 (MPH) directs the UNC Program in Nicaragua. (Photo by Anna Routh Barzin ’07)
The UNC Program in Nicaragua, directed by Dr. Sylvia Becker-Dreps ’08 (MPH), associate director of the Office of International Activities and an adjunct assistant professor in epidemiology, studies patients coming into health centers and emergency rooms with fevers. Researchers there are figuring out how to tell which ones are infected with Zika and whether they’ve had another tropical disease like Dengue before. Perhaps having antibodies to one of the Dengue strains is protective against Zika, or maybe it makes Zika outbreaks worse.
They’re following patients after they leave the health care setting to test how quickly the virus clears from blood and semen. They’re taking periodic blood samples so they can figure out when women were exposed and at what point during fetal development that exposure is the most harmful. So far it looks as if the second trimester is the worst time to get infected, said Dr. Matthew Collins, an infectious disease fellow at UNC who traveled to Leon.
The Nicaragua relationship has given UNC scientists a jump-start in studying the outbreak while it’s happening.
“Particularly when you’re talking about field projects like this one in Nicaragua, you need to get moving quickly,” Lazear said, “because this is a moving epidemic, and if you wait too long, you’ve already lost those early stages, and the timing is critical.”
In the months since the Zika-microcephaly link first became apparent, she said, “it’s become abundantly clear with a growing body of evidence that this is a virus that’s able to infect a developing fetus and cause damage and cause a range of birth defects. I think microcephaly was the first thing that was noticed because that’s a very dramatic presentation.”
Lazear expects that, over time, the list of additional developmental defects linked to this virus will grow, “just thinking about the sorts of developmental defects you can have with other viruses that are able to cross the placenta and cause birth defects.”
All of the insect-borne viruses — West Nile, Dengue, yellow fever and Zika — are spread by human travel. It happened with West Nile virus in 1999, Dengue in the ’80s and yellow fever with the slave trade in the 17th century. The problem is going to worsen as the world gets warmer, as populations encroach more on insect habitats and as global travel increases.
The collaboration and the systems the scientists are creating will be important far beyond this outbreak.
“Right now, we’re talking about Zika, but in a few years it’ll be something else.”
“It’s really a credit to the field how quickly we’ve learned so much about this virus that was essentially unstudied a year ago. The pace of discovery has just been astonishing. There’s a lot we don’t know, but there are a lot of people working on these questions, and I hope we’ll have answers for people before too long.”
Janine Latus is a freelance writer based in Chapel Hill.
Thanks for reading the Carolina Alumni Review
Carolina Alumni members, sign in to continue reading.
Not yet a member? Become one today.
