Ralph Baric: On the Front Lines of Coronavirus for Three Decades
Posted on March 13, 2020
Ralph Baric’s lab in UNC’s Gillings School of Global Public Health was among the first to receive SARS-CoV-2.
Ralph Baric was finishing his postdoctoral work in microbiology in the early 1980s just as the HIV epidemic was emerging. That might have been a logical direction for his research, but something else caught his attention: Coronaviruses.
“There was no real human pathogens,” he said. “But their replication strategy was uninvestigated and nobody knew very much about them, and so I wanted to go work on how this new group of viruses replicated in cells.

Baric
Baric found that coronaviruses jump species “pretty easily.”
“We wrote a couple of papers saying that these viruses have high potential as new emerging viruses, and then, like two to three years later, SARS emerged.”
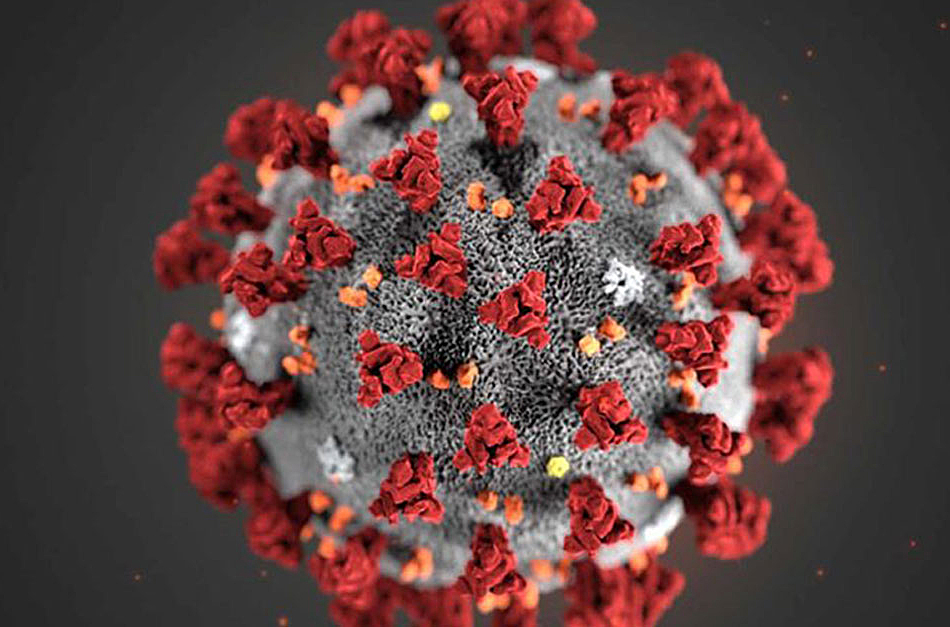
Severe Acute Respiratory Syndrome broke out in humans in China in 2002; it was a scare in the U.S. The virus that Baric calls SARS2 — and that is known more generally as COVID-19 in the recently declared global pandemic — has fundamentally altered life in much of the world, at least for the time being. Baric’s lab in UNC’s Gillings School of Global Public Health was among the first to receive SARS-CoV-2. It arrived in two sealed vials in early February.
Scientists who train for months just on the safety protocols for working with the virus — working in six-hour shifts because the batteries that power their respirators give out in eight — set about the tedious and agonizingly slow business of analyzing it.
“And then we begin to analyze growth in various cell types, and almost immediately we begin testing drugs,” Baric said.
On Tuesday, the Kenan Distinguished Professor of epidemiology, a 36-year UNC veteran, found in the checkout line of the building’s cafe, shook hands, stepped nonchalantly to the wall-mounted hand sanitizer and took a 40-minute break to talk about the differences between SARS 1 and 2, the arduous quest for a vaccine and his amazement that three new viruses have emerged during one scientific career.
Ralph baric
The Kenan Distinguished Professor of epidemiology also holds a professorship in microbiology and immunology and is a member of UNC’s Lineberger Comprehensive Cancer Center. He has 36 years at Carolina and is a fellow in the American Academy of Microbiology.
He holds an undergraduate degree in zoology and a doctorate in microbiology from N.C. State University, where he also broke four Atlantic Coast Conference swimming records. He did postdoctoral study at the University of Southern California School of Medicine.
Baric’s lab has been a magnet for government grant money: $21.4 million in 2012 and $10 million in 2013 to study potential virus infection treatments, and $6 million in 2017 to continue study on a coronavirus therapy that showed success in mice.
“And that’s only if you include the human coronaviruses,” he said. “If you include new emerging swine coronaviruses, there’ve been three of those as well since the beginning of the 21st century, so there’s six new emerging coronaviruses that came out of bats or other species to cause major outbreaks of disease with considerable loss either to human or animal populations.
“We had predicted that there were SARS viruses that are poised to move into human populations — the strains that we identified were not the strain that emerged in 2019.
“So it’s been a shock. I was shocked that MERS [Middle East Respiratory Syndrome] virus emerged in 2012 and caused human disease. And then a third one in 2019-2020.
“It’s kind of unprecedented. It suggests that there’s some kind of major change that’s occurred in global ecology that’s driving this event and coronaviruses are taking advantage of it. It could be that bat populations are being condensed. … It could be population density has reached a critical level that is just right for coronaviruses to start spreading more efficiently.
“Could be … you know, we almost have 1 billion elderly on the planet above 60, and coronaviruses like to replicate in old people. Probably a confluence of all those events. Coupled with global travel — almost instantaneous travel around the world.”
Talk about the differences between the first SARS and the current outbreak.
“There’s lots of viruses that jump between species — flu is the best example — which is a disease of birds and mammals” that then spills over into humans. “But there had not been any major human pandemic virus that was in our recent memory. It turns out the contemporary human coronaviruses — of which there are four that you’ve been infected with and I’ve been infected with — they emerged 100 to about 800 years ago. And there’s no recorded information about what disease they caused or whether they caused any disease. And even if they caused disease, it probably would have been written off as flu.
“SARS(1) had multiple vulnerabilities that allowed us to control it by public health intervention methods. We knew the virus had an animal reservoir, and it was civets and raccoon dogs, and they were in the open markets, and they had strains that were 99.8 percent identical, that could spill over and infect people. So if you culled the animal reservoir by killing all the civets and raccoon dogs, then that transmission route’s been ended.”

Baric’s lab, including about 15 people who are certified to work at the biological safety level required for the virus, is working toward a vaccine.
The second measure, Baric explained, was barrier nursing techniques — use of masks, gloves, gowns, etc. — “which almost always are a little sloppy, and so hospitals are caught off guard when a new emerging virus sweeps through. And then they instantly ramp it up, and that helped control the SARS outbreak.
“And the third is, people didn’t transmit SARS until they were really sick. They didn’t transmit until 24 to 36 hours after they were sick, clinically ill, so they never transmitted when they were asymptomatic or had mild disease, only when they really got sick, and everybody that got infected got really sick.
“SARS2, we don’t know what the animal reservoir is, so we can’t cull the animals. They implemented barrier nursing in China, 1,700 health care workers got infected — not sure why.”
And third, he said, “SARS2 can be transmitted asymptomatically and in mild cases, so community spread is rampant.”
Baric’s lab, including about 15 people who are certified to work at the biological safety level required for the virus, is working toward a vaccine. He talked about that process, which he said will take between a year and a year and a half.
“The first milestone is to demonstrate that the vaccine candidate elicits an immune response that we think is protective … that the vaccine’s safe, it doesn’t induce immune pathology, for example, or it doesn’t cause disease enhancement. Some vaccines can go terribly wrong. One concern with this new virus is that some of the SARS coronavirus vaccines that were developed in 2003 went horribly wrong: They induced in animal models human disease — not in humans but in animal models.
“The next step is to demonstrate that the vaccine candidate actually protects against lethal challenge. So you need mouse models or other animal models of human disease, and once that data’s been demonstrated, then you typically need a second animal model like a primate that you have to demonstrate efficacy in, and they don’t have to be done linear, they can be done simultaneously — especially depending on the urgency. So in a case like this — where we’re bordering on a global pandemic with 3.4 percent mortality rates, right? — you start everything simultaneously.
“That helps condense the amount of time between candidate development and actual Phase 1 trials in humans. So the time it takes to make a candidate, for example, is probably two weeks. There are vaccine candidates against SARS2 all over the United States — most major research laboratories already have some.
“Then, companies have their own vaccine platforms that they’re pursuing. So there’s probably 25 to 30 different vaccine platforms that are under development.

Congress has appropriated an emergency $8 billion fund to fight the impact of the coronavirus. Baric said he understands that a “big block” of that money will go to the National Institutes of Health and that NIH is enabling labs to convert existing grants to focus on the virus.
“Then you go to Phase 1 trials in humans. That’s usually an escalation study, where you put more and more of the vaccine in a person and you see whether [there are] any adverse responses at the site of vaccination, did they tolerate the vaccine well. And then they look at immunologic features — did it induce an immune response, did it make neutralizing antibodies. …
“ ’Course those people [in the trials] are likely to go out into the world, and if the virus cycles through again next year, we get to see if the vaccine worked.”
As the world waits, naturally people want to know the prospects for the spread of the virus.
“There’s two camps: One camp argues this is the major peak of disease and we’ll have a minor peak of disease next year. The other camp argues that this is the minor peak and the big peak is coming next year.” Baric laughs. “And then the third camp says it either won’t happen or it will be the same.” And, with an exasperated laugh, “Any possibility is right now possible.”
Congress has appropriated an emergency $8 billion fund to fight the impact of the coronavirus. Baric said he understands that a “big block” of that money will go to the National Institutes of Health and that NIH is enabling labs to convert existing grants to focus on the virus. He talked at length about the best ways to use money.
“It’s a mistake to concentrate too much money into one laboratory. There’s a scientific community of individuals who have elegant expertises around the country that have been focused on other pathogens or other disease models, and this SARS2 outbreak provided an opportunity for people to integrate that knowledge set into the field of coronavirology. So I would really like to see that happen.
“More people engaged brings more expertise, more insight, more creativity. The advantage we have, of course, is experience and knowledge of the field, and we’ve built resources for 30 years that no one else has.
“But that doesn’t mean that I always have the best questions. There are other people who have insight, and it’s important that they get engaged. So I was pretty elated at the way NIH set it up so that people could convert existing grants. … I think that’s great.” Of the new money that NIH could get, he said, “Exactly how that will break down and trickle down through the system is unclear.”
What would you do with a windfall?
“We have a major effort in terms of developing drugs against emerging coronaviruses — not only just emerging, but any coronaviruses — so we’re really focused on developing broad-based drugs that would work not only against the contemporary strains and the known epidemic strains, but — the animal reservoirs are filled with strains that are poised for cross-species movement to humans, and I mean poised meaning that they can already use the human receptors for entry and they can already grow in the primary cells of our lungs. They just aren’t because random chance hasn’t brought a human into contact with the right bat that happened to drop a guano thing … to a person that got them infected.
Baric found that coronaviruses jump species “pretty easily.”
“But they’re filled with SARS- and MERS-like strains that are quite different antigenically from the original 2003 strain and the 2020 strain that could cause outbreaks in human disease. So what we really need are broad-based drugs and vaccines on the shelf, and that’s what our major goal has been for quite some time.
“If you really want to develop a broad-based drug against all SARS-like viruses, you want to have the bookends — the most distant ones, [and] you want to have something in the middle. And the hypothesis is, ‘OK, if the drug works against the most anti-genetically distinct ones and one or two in the middle, then it would probably work against the unknown that emerges in the future.’ That’s the idea.”
Asked what he recommends people do to mitigate the spread of the virus, Baric pointed to history.
“Everywhere in the world where they implemented draconian public health measures to stop the spread, where people come together, has had low-level linear increases in a number of cases. Hong Kong, which is right next to China and during the SARS(1) outbreak had 600 to 700 cases, immediately put in draconian methods. They closed schools, they closed universities, they told people to work from home, they prevented public gatherings at sporting events or other things, they told them to stay off the streets.
“If you want to blunt the scope of the outbreak, you have to [minimize gatherings]. The data is clear — in fact, the data is clear all the way back to [the flu pandemic of] 1918.”
“You look at Hong Kong, they usually see two or three cases a day. You look at places that didn’t, especially nations that said it’s ‘not a problem’ — the most dangerous three words, it’s ‘not a problem’ — the coronavirus, it gets a little smile on its face when it hears the words ‘it’s not a problem.’ It spreads rapidly in silent transmission networks.
“Right now we have a big flu season; most people who show up at the hospitals are being treated for flu. There was certainly no diagnostic test that was widely available in January and February and even now. So they’re treated with Tamiflu or something, which is worthless — it doesn’t do anything. Eighty-three percent of the SARS2 infections are mild, asymptomatic, moderate disease. You get better in a few days, but for eight to 10 days you are transmitting high titer [antibody concentration] virus to everybody around you. And those silent transmission networks are deadly because it takes up to 14 days before they develop clinical disease, and they will shed virus for four or five days before that. So you have these long transmission windows that are occurring that are allowing the virus to spread in communities in an insidious manner.
So, minimize gatherings?
“If you want to blunt the scope of the outbreak, you have to. The data is clear — in fact, the data is clear all the way back to [the flu pandemic of] 1918, where Philadelphia had a giant parade and had massive numbers of cases, and St. Louis canceled everything and said we’re not doing any kind of public gathering. And their case rate was really low, and Philadelphia was through the roof.
“If you really want to control it, you’ve really got to do these really draconian measures where you say, ‘Time to go home.’ The problem, of course, comes in the impact of that to the economy, the impact on people’s lives — can they keep their house payments going, can they afford food, what kind of support is available from the government to handle that as part of a global public health emergency? Or do you let it burn through the population? So, tough decisions. Or easy decisions, depending on your point of view.”