From the Ashes, a Cure
Posted on Jan. 21, 2022
(Grant Halverson ’93)
Jude Samulski’s 40-year gene therapy odyssey has led to beneficial treatments for kids with serious single-gene disorders. This is the story of how it happened — but almost didn’t.
by Mark Derewicz
Jude Samulski, a 30-year-old gene therapy wizard, awakes in a quaint English inn, ambles to the breakfast table and a chipper English woman strikes up a conversation he’ll never forget.
Serving eggs and too much sausage, she asks, “So what brings you to Cambridge?”
Samulski says, “Oh, I’m here for a meeting. I work on viruses.”
“I see. Viruses?”
“Well, we’re trying to figure out how to use viruses for gene therapy.”
“Oh, I see. My son has a genetic disease.”
Samulski is surprised. It is the mid-1980s, gene therapy is barely a thing, and it’s not every day you meet someone with a child with a rare disease.
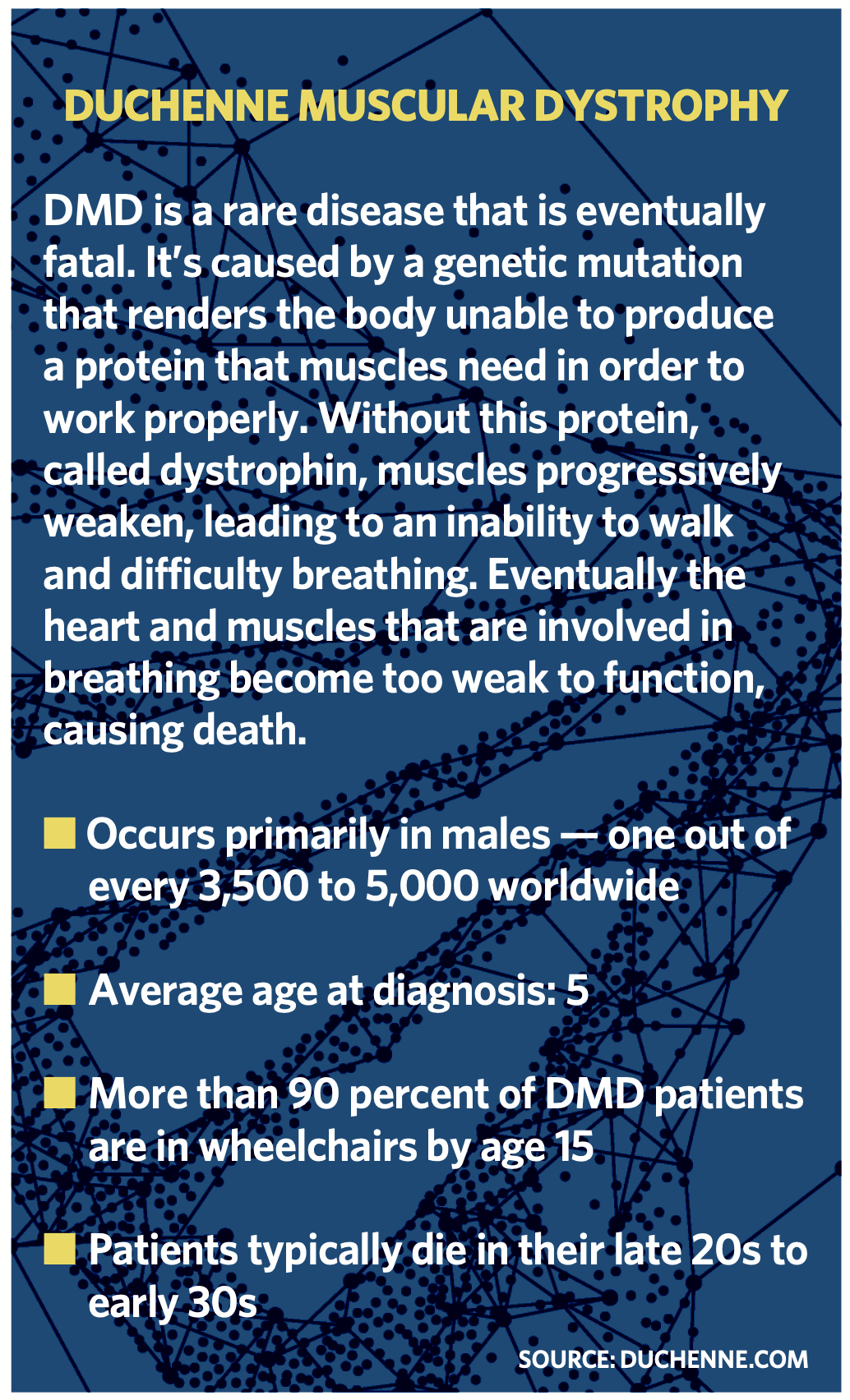
“He has Duchenne muscular dystrophy,” she says.
Samulski doesn’t know much about the condition. He has no idea that other scientists are just now discovering the single faulty gene responsible for the disease.
Samulski asks, “What are doctors doing for your son?”
“Nothing,” she says. “Nothing can be done. We’re building a bedroom for him, downstairs.”
Samulski looks her in the eye when she pauses. She says, “You understand? So our boy doesn’t need to climb stairs.”
 Samulski nods politely, but inside he’s horrified. How could medicine still be so archaic that all we can do for these kids is make their lives a little easier, make it so they don’t have to climb stairs?
Samulski nods politely, but inside he’s horrified. How could medicine still be so archaic that all we can do for these kids is make their lives a little easier, make it so they don’t have to climb stairs?
When Samulski left breakfast for the meeting, he had no idea he would later come to Carolina to start a gene therapy center and found companies worth billions of dollars — such as Bamboo Therapeutics and AskBio — that would help kids with Duchenne muscular dystrophy. And he had no idea he’d befriend a boy named Conner Curran and his parents, who in 2017 would be the first to bravely enroll their son in a Duchenne MD clinical trial using a gene therapy Samulski and colleagues would create.
Four years after his initial treatment, Conner runs toward Samulski, and the scientist, now 67, thinks of that mother in England. And he thinks of a father from Texas — a man who came to the rescue out of nowhere when the gene therapy field was in crisis two decades ago and research around the country was being shut down.
Into the unknown
From his earliest memories, Samulski was attracted to pushing boundaries. The youngest of nine kids, he preferred Star Trek to Star Wars, intrigued by the idea of boldly going where no one has gone before to discover things nearly impossible to imagine. This led him to science. When Samulski was a Clemson undergrad, his virology professor encouraged him to find a job at the best lab possible. In 1976, freshly graduated, he got a job as a research associate in Dr. Sherman Weissman’s lab at Yale, where researchers were figuring out the complete nucleic acid sequence of simian virus 40, which has the potential to cause tumors in humans.
Weissman, like all great academic scientists, was part mentor, apt to dispense truths young scientists needed to hear.
“He told me, ‘As long as you stay in my lab, you will pursue my ideas,’ ” Samulski said. “ ‘So you need to find a young investigator just starting their lab, a place you can work side by side with them to pursue your ideas.’ ”
Samulski scoured the scientific landscape for such investigators and came across Nic Muzyczka, who had just started a lab at the University of Florida. Muzyczka had previously worked as a postdoctoral fellow in a lab run by a couple of Johns Hopkins scientists who had won a Nobel Prize on recombinant DNA — shorthand for using enzymes to cut and paste together DNA sequences from different species, such as bacteria and viruses, inside the same cell. New postdocs usually lead the lion’s share of experiments and depend on sharp graduate students. Samulski contacted Muzyczka, interviewed for a position, was hired and joined the Florida lab as a 23-year-old virology graduate student to create recombinant DNA.
“We were like a family,” Samulski said. “We really clicked, and all of us were gung-ho about our projects.”
The Muzyczka lab studied how viral DNA could be re-jiggered to become a harmless shell of a virus that could still move like a virus and “infect” cells without causing harm. This viral vector would simply be a delivery truck, delivering whatever the researchers wanted to put inside the vector, such as a therapeutic agent or even a working gene.
“Back then, we did experiments in special suits, fully gowned up and behind double-locked doors,” Samulski said, smiling. In hindsight, such precautions were not necessary. “But it really was like being in the space program. Everything was new. It was so exciting. I definitely drank the cutting-edge science Kool-Aid.”
At UF, Samulski led the creation of adeno-associated virus vectors. AAVs are small viruses that infect primates, including humans, but are so harmless that our immune systems barely respond to them. This is good, because they can be used as a vector for a therapy. The last thing you’d want is the body to recognize a harmless gene therapy vector as a pathogen and attack it, as other researchers would find out.
Samulski took his AAV vector work with him for postdoctoral work at Princeton, where he figured out how to fit recombined DNA sequences into an AAV vector and send it into human cells in a dish. He patented this work in 1985.
As the 1990s crested, the buzz surrounding gene therapy got loud. The concept was so easy to explain — swap out a bad gene with a new one to cure kids — that it seemed too good to be true. And then, in 1999, it was.
This in a nutshell is the original idea of gene therapy: The AAV vector is like an Amazon truck. The Amazon package is the healthy recombined DNA. The researchers needed to make sure that the truck delivers the package exactly where it needs to go and only where it needs to go. And they needed to make sure the recipient accepts the package, knowing that the recipient lives in a neighborhood with a serious crime watch program called “the ever-vigilant immune system.”
Baby and the bathwater
Samulski is not a medical doctor. He did not get into science to run clinical trials or see patients. In his first tenure-track faculty position at the University of Pittsburgh, he tested his basic AAV vector in various lab experiments before Carolina came calling in 1993.
Bill Marzluff, the UNC School of Medicine vice dean for research at the time, and Carolina scientist Dr. Ric Boucher, a pioneer in cystic fibrosis research, recruited Samulski.
Marzluff had been a postdoc in the lab next door to Muzyczka’s lab before Samulski arrived, and he knew Samulski’s postdoc adviser.
“Ric heard Jude give a talk at a conference and was convinced Jude was determined to make this [AAV vector] work, no matter how long it took,” Marzluff said.
Marzluff and Boucher traveled to Pittsburgh for an initial introduction, a rare show of genuine interest, and Samulski was impressed. So were Marzluff and Boucher.
“Jude’s lab had already discovered that when a mammal is infected with AAV, the virus integrates into the mammal DNA at a specific place where it does no harm,” Marzluff said. “That impressed me.”
Still, Samulski said, “I told them, ‘If you’re looking for someone to put this vector in patients, you have the wrong person. But if you’re looking for someone to figure out the science — to really understand if and how this works, knowing it might take 20 more years —then I’m your guy.’ ”
When Samulski visited Carolina, Marzluff and Boucher introduced him to Eric Munson, head of UNC Hospitals at the time, who committed $1 million to help set up a facility to make clinical-grade AAV vectors. Marzluff and Boucher also helped secure $500,000 from the N.C. Biotechnology Center to build a production facility because, no matter who ran clinical trials, they’d need product.
“If we could not produce a lot of AAV vectors to treat 40,000 people with a disease, then it wouldn’t matter if we could treat a mouse,” Samulski said.
Samulski’s star rose throughout the 1990s as his lab honed AAV technology for human diseases such as hemophilia and muscular dystrophy, and he founded the UNC Gene Therapy Center. For several years, according to Marzluff, UNC clinicians didn’t think gene therapy would work.
“Unfortunately, Jude’s lab quickly proved his method did not work for cystic fibrosis, which was Ric’s main focus,” Marzluff said. “The CFTR gene that is faulty in CF patients was simply too large to package inside the AAV.” It wouldn’t work as a CF treatment. But that didn’t mean AAV gene therapy wouldn’t work for thousands of other rare diseases.
As the 1990s crested, the buzz surrounding gene therapy got loud. The concept was so easy to explain in the media — swap out a bad gene with a new one to cure kids — that it seemed too good to be true. And then, in 1999, it was.
Teenager Jesse Gelsinger died during a small University of Pennsylvania clinical trial for a rare disease called ornithine transcarbamylase deficiency syndrome. Gelsinger’s condition when he enrolled had not been life threatening, and there was no question the clinical trial led to his death. Just like that, the hype and hope were gone. The federal government halted all gene therapy clinical trials. An investigation into the University of Pennsylvania clinical trial found problems with how it had been administered. Researchers were accused of hubris, of playing God, even. Penn was sued, settled with Jesse’s parents, and then shut down its gene therapy program. Even the term “gene therapy” became taboo. Projects around the country were shelved.
Teenager Jesse Gelsinger died during a small clinical trial for a rare disease. There was no question the clinical trial led to his death. Just like that, the hype and hope were gone.
“The field was dead,” Samulski said. “NIH funding dried up.”
Samulski managed to keep the center going with a few grants, but the research was conducted in the lab; there were no clinical trials. It looked like the center’s days were numbered, even for basic research, even though Samulski’s approach was not the same as Penn’s.
A guardian angel
There are two main gene therapy camps. One investigates the use of adenoviruses as the means to deliver working genes directly into cell chromosomes, where genes reside. Adenoviruses can cause common illnesses such as colds, bronchitis, pink eye and pneumonia. Samulski pioneered the other camp, which uses adeno-associated viruses. Not only does the immune system play nice with AAVs, but Samulski developed his vectors to deliver payloads outside of chromosomes, thus limiting the chance the vector will disrupt other genes. There are other differences, but those are two big ones.
The Penn researchers and colleagues did attempt to render the adenoviruses and their payloads harmless. But the Gelsinger case showed adenovirus vectors could still trigger such a massive immune response that doctors could not tamp it down, which is what lead to Gelsinger’s death.
“A lot of people could not distinguish between the two main gene therapy delivery systems,” Samulski said. “Maybe we didn’t do a good enough job communicating the differences. Regardless, everyone got sidelined for that very unfortunate failure. But what happened to the field would be like a cancer drug failing, and then every similar drug was canceled.”
With the burgeoning field in tatters in 2000 and Samulski’s research funding running out, a Texas millionaire by the name of Trip duPerier appeared in Chapel Hill. His son had Duchenne muscular dystrophy. Bound to a wheelchair and breathing and eating through tubes, the boy would never benefit from a miracle drug that might come online in the future.
That’s because gene therapy for Duchenne MD might stop muscle deterioration, preserve what remained and improve some muscle function, but it would not bring back nearly enough lost muscle function to help duPerier’s son, who could not walk or breathe on his own. Still, Trip wasn’t in it for his son.
DuPerier told Samulski, “I just don’t want parents to go through what I’ve been through. I just know you can do this. I believe in the science.”
“Trip asked us what we needed,” Samulski said. “We showed him everything we had done, the facilities and the people here. And we told him that to continue it, we needed funding.” DuPerier cut a check for $3 million before he flew back to Texas.
“Trip was like a guardian angel. He just appeared,” Samulski said. “It was … just remarkable.” (The Review could not reach duPerier for an interview.)
On the heels of duPerier’s visit, Samulski contacted the Muscular Dystrophy Association about funding opportunities. The MDA encouraged Samulski to start a company focused on a treatment for Duchenne MD and other rare-disease AAVs.
In 2001, along with attorney Sheila Mikhail and Carolina pharmacy professor Xiao Xiao, who had been a grad student and postdoc in Samulski’s lab, Samulski co-founded Asklepios BioPharmaceuticals (AskBio). It was Xiao’s work that showed it was possible to create a miniature version of the dystrophin gene product so it could fit inside an AAV vector to be safely delivered into muscle. Xiao led experiments showing the therapeutic value of the AAV vector in mice and then showed how it rescued muscle strength in dogs.
“Jude’s lab just kept coming up with these incredible tricks to make AAV better and safer. It’s absolutely amazing. I remember he gave a talk telling us about how he was going to do it, and damned if he didn’t do exactly what he said he’d do, and it worked.”
— Bill Marzluff
With duPerier’s funding in hand, Samulski would end lab meetings by saying, “Okay everyone, imagine Trip’s son is your son.”
In 2004, AskBio secured a $1.6 million grant from the Muscular Dystrophy Association. Still, AskBio was a small startup, and for the first decade, none of its founders were paid. All grants and investments paid staff and covered facility costs.
Thanks to the animals
Carolina is a leader in animal research. To some, that shouldn’t be a source of pride, but without animal research very little, if any, biomedical research would turn into treatments for people.
“UNC’s dominance in this is a big reason why I came here,” Samulski said.
“Animal models that mimic human diseases, such as muscular dystrophy, hemophilia and CF, make it possible to introduce our research into complex organisms. We don’t do this lightly. We do this work as carefully and intentionally as possible. But it must be done to validate our work and to learn every single thing we need to learn before human trials.”
Samulski’s team showed how Duchenne MD mice gained and sustained muscle function over time. The researchers homed in on proper dosing, side effects and how the treatment works when given at specific ages. They studied everything — weight gain, immune response, fever, blood chemistry, organ toxicity.
This painstaking research took years, but the therapy looked safe and effective, leading AskBio to submit to the Food and Drug Administration an application for “Preliminary Investigation of a New Drug,” or a pre-IND. At this step, the FDA reviews data and advises the researchers on what they need to do before submitting a larger IND package that includes all data the scientists have ever documented. During pre-IND, the FDA also might advise the researchers to, say, focus on treating four-year-olds but not infants.
Then scientists submit a toxicology bio distribution package, showing what happens to organs when the therapy is given at proper doses and at high doses. They document immune responses.
“Basically, we see if we can create a problem,” Samulski said. “And if so, what the problem is and how to avoid it.” When all of that goes well, scientists submit yet another application for a small clinical trial, explaining exactly how they would treat a small number of patients with the primary goal of investigating safety, while also documenting any potential benefit.

“The whole thing really has been like a moon shot,” Samulski said. “Back in the 1990s, no one knew what the best gene therapy approach would be. To our benefit, we picked the one that went to the moon. But we could not have predicted that from the beginning.” (Grant Halverson ’93)
“This is an extremely important collaboration with the FDA, and we’ve had a remarkable interaction with them,” Samulski said. “They realize these rare, so-called ‘orphan diseases’ are typically not very popular and research is not well funded. But they also know that if you count all the people in the world with an orphan disease, the total number would be the third most populated country in the world.”
End game
For Samulski, this gamut to get an AAV into clinical trials for Duchenne MD and spinal muscle atrophy began last century in his lab at Chapel Hill. It included the creation of AskBio and then the creation of an AskBio spinout company, Bamboo Therapeutics, which originally focused on Duchenne MD.
Henrik Dohlman, UNC’s chair of pharmacology, said, “Jude is the rare scientist who has succeeded in moving from purely curiosity-driven lab research to real-world, life-saving treatments. The fact he brought, directly and indirectly, hundreds of biotech jobs to the Triangle only adds to his legacy.”
Gene therapy is now the fastest growing area in therapeutics, Dohlman said.
In 2016, pharmaceutical giant Pfizer purchased Bamboo to get the treatment into clinical trials.
Trip duPerier’s generosity wouldn’t directly help his son, but it would help other families and kids like Conner Curran.
In 2017 at Duke, Conner watched a video as the clinical research team put billions of AAV vectors into his blood over the course of two hours.
“It was a scary moment for us,” Samulski said. “But we did everything we could do to get us here.”
Conner ate a pickle and said he wanted to go swimming when they were done.
The clinical team closely monitored Conner for days. Within a few weeks, he was running up the stairs and walking two miles to the local bagel shop. He could do neither before the treatment. Conner and other boys in the trial got temporarily ill, an immune reaction to the treatment. So Samulski and colleagues created what they hope is a solution to stop any reactions. They’ve tested it in animals. So far, so good.
But even without that fix, Conner and the other boys have been doing well for more than three years, and Pfizer has submitted that data to the FDA.
Marlzluff said, “Jude’s lab just kept coming up with these incredible tricks to make AAV better and safer. It’s absolutely amazing. I remember he gave a talk telling us about how he was going to do it, and damned if he didn’t do exactly what he said he’d do, and it worked.”
In September 2021, Samulski said, “I just talked to Conner last week. He is a great kid. And his family is remarkable. Being part of this has been truly amazing.
“The whole thing really has been like a moon shot,” Samulski said. “Back in the 1990s, no one knew what the best gene therapy approach would be. To our benefit, we picked the one that went to the moon. But we could not have predicted that from the beginning.”
AskBio made headlines in 2020 when Bayer AG bought the company for $2 billion with options for $2 billion more if AskBio meets certain milestones. AskBio scientists now are working on AAV-based treatments for Huntington’s disease, Friedreich ataxia, Parkinson’s disease, respiratory conditions and extremely rare genetic diseases. And because genes play such a major role in common diseases, AskBio is researching solutions for certain kinds of heart diseases, chronic pain, obesity and addiction.
Samulski isn’t finished. He’s been at this for 40 years and each year brings new insights, new problems to solve and new excitement. Yet now that AAV gene therapy is in clinical trials and, in two cases, FDA-approved, he does think back a little more than he used to. He thinks of that mother in England. He thinks of Conner, his parents and other families dedicated to exploring what’s possible. And he thinks of Trip duPerier.
“These kids and these parents, they really are the reason we do this,” Samulski said. “Trip duPerier and I are still fantastic friends. I can truly say his magnanimous gift is the sole reason our work broke free. Without him, we would not be here.”
Mark Derewicz is director of research news for UNC Health and a freelance writer living in Chatham County.
Thanks for reading the Carolina Alumni Review
Carolina Alumni members, sign in to continue reading.
Not yet a member? Become one today.